Safe use of insulin for adults admitted to hospital - Medicines Reconciliation
Part 1 - Medicines Reconciliation (Meds Rec) on admission
This blog is the first in a series outlining risks relating to insulin prescribing and administration for adults in hospital, and at discharge and aims to provide good practice points to minimise these risks.
Key messages
- Errors involving insulin can cause serious harm to patients. Accurate medicines reconciliation is essential to maintain patient safety.
- For general advice on insulin, clinical staff are advised to follow the NHSGGC ‘Key Insulin Safety Tips’ which can be accessed via Diabetes, Inpatient Prescribing FAQs for Junior Doctors.
- Follow the five medicines reconciliation steps below.
Medicines Reconciliation (Meds Rec)
|
Always use at least two sources to confirm a drug history: remember to involve the patient, who will often be the most accurate source of insulin dose information. |
-
Confirm the patient is on insulin
- Remember, ALL patients with type 1 diabetes will be prescribed insulin.
- Insulin can sometimes be ordered less often than oral medication depending on the patient’s regimen and dosage and may therefore appear further down the Emergency Care Summary (ECS) or appear not to have been ordered for several months.
- Always check the full ECS list and confirm with a second source, ideally the patient/carer.
-
Confirm the brand of insulin
- Insulin should ALWAYS be prescribed by brand. Prescribing by brand reduces confusion as staff/patients can often be unfamiliar with generic names for insulin
- Insulins with the same generic name may have a different insulin release profile. For example:
- NovoRapid® and Fiasp® brands both contain insulin aspart. However, as Fiasp® is faster acting, they are not inter-changeable and need to be taken within different timeframes in relation to meals.
- Be cautious of insulins with similar names. For example:
- Humalog® contains insulin lispro (short-acting) but Humalog Mix 25® and Humalog Mix 50® are biphasic preparations containing differing ratios of insulin lispro (short-acting) AND insulin lispro protamine (intermediate-acting). Humalog® is given with meals, usually within a basal bolus regime in addition to a long acting insulin (e.g. Levemir®, Tresiba®). Humalog Mix 25® or Mix 50® is usually administered twice daily with breakfast and evening meal.
- ECS shows the brand prescribed in primary care, however, medicines imported from ECS into the Orion Medicines Reconciliation/Immediate Discharge Letter (MR/IDL) system on Clinical Portal, can sometimes automatically convert to their generic name. Recent updates to Orion should prevent this but if this occurs, access ECS directly to determine the brand name and endorse it during the Medication History step of the Meds Rec review. If the brand name is not clear on ECS, check with the patient/carer.
-
Confirm the concentration of insulin
- A number of high concentration insulins are now available. Standard concentration insulin is 100 units/ml and high concentration insulin is 200 units/ml or 300 units/ml (see Figure 1 below).
- If patient is on high concentration insulin before admission, ensure this is clearly documented on the Orion MR/IDL system to ensure accurate prescribing.
- Figure 1. Examples of high concentration (300 units/ml) versus standard concentration (100 units/ml)


-
Confirm the device
- Insulins are available as vials, cartridges (for use in refillable pen devices) or disposable pre-filled pens.
- It is good practice to include the patient’s insulin needles on Meds Rec documentation. This can be done when importing the ECS list onto the admission medication review on Orion.
- This information is helpful to assist patients to continue to self-administer their insulin (under nurse supervision) while in hospital and facilitate appropriate supplies on discharge.
Subcutaneous Insulin Pumps
- All patients admitted to hospital using a subcutaneous insulin pump should be promptly referred to the inpatient diabetes team.
- If a patient usually uses a continuous subcutaneous insulin pump and is unable to self-manage during admission, they should be switched to a variable rate intravenous insulin infusion (VRIII) in the first instance (See NHSGGC Diabetes, Inpatient Prescribing FAQs for Junior Doctors).
-
Confirm dose and frequency
- If dosage information is available on ECS and/or the Orion MR/IDL system it may not be the patient’s current dose.
- It is essential that the dose is confirmed with a second source on admission to hospital e.g. patient, carer or district nurse.
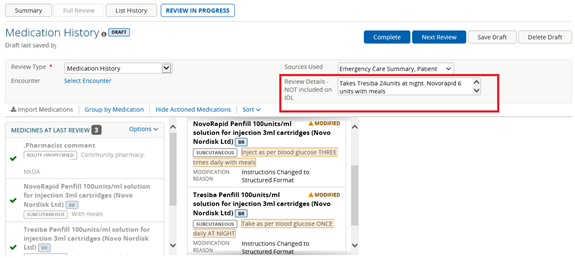
- When completing the medication history on Orion, DO NOT document the patient’s current dose with the drug entry. The dose of insulin should be specified in the “Review Details” box in the top right hand corner of the screen (by clicking the
 icon). This allows for accurate documentation of the admission dose history, but prevents inaccurate information being carried over on discharge when the IDL is generated.
icon). This allows for accurate documentation of the admission dose history, but prevents inaccurate information being carried over on discharge when the IDL is generated.
See example below (use zoom function to enlarge image and if using a mobile device, switch to landscape):
Refer to other blogs in the insulin safety series:
Safe Use of Insulin for Adults Admitted to Hospital – Summary of Blog Series
Safe use of insulin for adults admitted to hospital - Prescribing
Safe use of insulin for adults admitted to hospital - Administration
Safe use of insulin for adults admitted to hospital - Discharge
|
Remember: Patients with type 1 diabetes or previous diabetic ketoacidosis (DKA) should always receive their long acting insulin while an inpatient (unless advised by the inpatient diabetes team). Missing any insulin can lead to development of DKA. |
Published 07/03/2023. Link to guideline updated 08/09/23. Medicines Update blogs are correct at the time of publication.
If you would like to subscribe to Medicines Update or provide feedback on the blogs, email medicines.update@ggc.scot.nhs.uk.
Follow Medicines Update on Twitter @NHSGGCMeds
